What is the difference between venous and arterial leg ulcers?
Studies show that around 3.8 million people require wound treatment in the UK.[1] This figure represents a 71% increase from 2012/2013, with pressure, venous and arterial leg ulcers consistently being the most treated wounds by the NHS each year.[2]
Leg ulcers are common in people over the age of 65 and can have an extremely negative impact on a person’s overall quality of life. People often report pain, discomfort, reduced mobility, anxiety, depression, and unscheduled hospital visits as the key consequences of living with a leg ulcer.[3]
What are leg ulcers?
A leg ulcer is defined as ‘a break in the skin on the lower leg, which takes more than 4-6 weeks to heal.'[4]
The most common types of leg ulceration are venous and arterial.[5]
Although veins and arteries are the primary blood vessels in the body, they perform vastly different functions.[6] Understanding the underlying cause of a person’s leg ulcer is important for ensuring that the appropriate treatment plan is implemented.
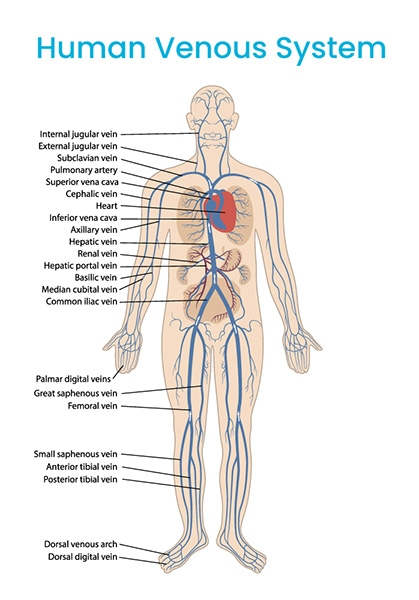
What are veins?
The veins are blood vessels that form part of the venous system. The venous system is a network of veins that link to other blood vessels and organs in the body.
The primary function of the veins is to carry oxygenated blood back to the heart.[7]
There are two different types of veins: superficial and deep veins. Although both types are closer to the skin than the arteries, superficial veins lie directly under the surface.
Deep veins are located deeper in the body, near the bones around the legs and feet. Deep veins are operated by the calf muscle pump during movement.[8]
Why do venous leg ulcers occur?
Venous leg ulcers can occur because of chronic venous insufficiency (CVI).
The veins have one-way flaps of tissue known as valves. When the valves are working properly, they prevent the backflow of blood into the lower limbs.[9]
CVI occurs when the valves are damaged and cannot function correctly. This means that the blood is unable to flow upward properly and begins to flow downward. This is known as venous reflux. This can lead to blood pooling and increased venous pressure in the lower limbs.
What are the main risk factors for venous leg ulcers?
The risk of developing a venous ulcer increases with other factors:
• Age – the valves in the veins become weaker as the body ages.
• Obesity – being overweight increases pressure in the lower limbs.[10]
• Varicose veins – swollen and enlarged veins.
• Deep vein thrombosis (DVT) – is caused by a blood clot forming in the deep veins of the body, most notably in the legs.
• Smoking – cigarettes reduce the oxygen levels in the blood, which can have a detrimental impact on venous function.[11]
• Lower limb surgery – surgeries like hip replacements can cause temporary mobility issues, which can impact blood flow.
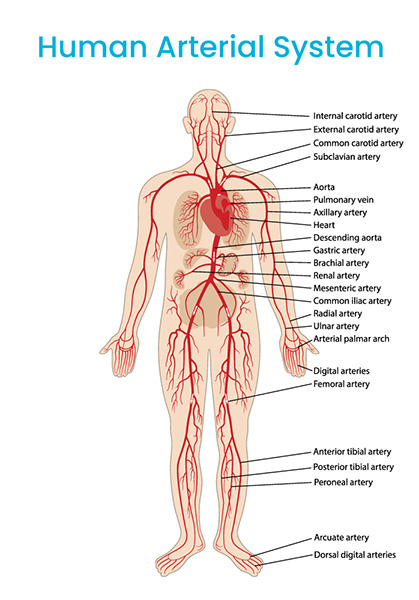
What are arteries?
The arterial system is tasked with distributing oxygen and nutrient-rich blood to the tissues and organs.[12]
The arteries are the strongest blood vessels. The arteries are composed of three layers that can withstand the strong pumping action of the heart. This enables the blood to flow through the arteries at a consistently high pressure.
There are three main types of arteries: elastic, muscular and arterioles.
The elastic arteries are made up of more elastic tissue and are those closest to the heart. Elastic arteries can tolerate blood surges and sustain a relatively consistent pressure gradient because of their flexibility.[13]
Muscular arteries contain smoother muscle cells than their elastic counterparts. This allows them to draw blood from the elastic arteries and distribute it around the tissues and organs.[14]
The arterioles branch off the larger arteries into the capillaries, which are the small blood vessels that they disseminate blood to and trade oxygen with. The arterioles are also responsible for regulating the body’s blood flow.
Why do arterial leg ulcers occur?
Arterial leg ulcers, sometimes known as ischemic ulcers, occur because of reduced blood flow in the arteries. This happens when a type of plaque called atheroma builds up in the arteries. This plaque is made up of fats, cholesterol, and other substances.
This plaque leads to stenosis (a narrowing of the affected artery), which decreases the blood supply in the arteries. When the supply of blood decreases, so too does the supply of oxygen.
When the tissue fed by a particular artery is deprived of oxygen and nutrients, it begins to break down. This disintegration of tissue can lead to an arterial leg ulcer in the affected area.
What are the main risk factors for arterial leg ulcers?
• Age – arterial function diminishes with age.
• Obesity – being overweight can lead to a build-up of fatty material in the arteries, which can cause clogged arteries and even a heart attack.
• Diabetes – can affect the lining of cells in the blood vessels, which can impact arterial blood flow.[15]
• Hypertension – can cause excessive venous pressure, which can exacerbate the effects of arterial disease.[16]
• Physical inactivity – caused by mobility issues or a more sedentary lifestyle makes it more difficult to maintain a healthy weight. This can increase the risk of hypertension.
What are the key differences between the two?
| Question | Venous | Arterial |
|---|---|---|
| Where is the ulcer located? | Gaiter area. Usually on the inside of the leg, particularly around the ankles.[16] |
Lateral compartment of the leg. Arterial ulcers normally occur over the bony prominences of the foot such as the heels and toes.[17] |
| What does the ulcer look like? | Superficial wound. Size can range from small to large. Irregular and sloping edges. Sometimes shows the presence of contact dermatitis and varicose eczema. Lipodermatosclerosis. Swelling and oedema. Sloughy. |
Full-thickness wound. Blanched and taut skin. Minimal hair on the lower leg. Gangrene. Minimal exudate. Necrotic tissue. |
| What does the ulcer feel like? | Heaviness in the lower limbs, especially around the ankles. Persistent throbbing and pain. Aches. |
Intermittent claudication (pain in the thigh, buttocks, and calf when walking). |
| What are the main treatments for the ulcer? |
Compression therapy. Elevation.
|
Surgery may be required to clear out a build-up of plaque in a leg artery (endarterectomy). An angioplasty is often performed to treat the blockage in the leg arteries. It involves using a balloon or stent to stretch the artery. This can improve blood flow and reduce the symptoms associated with arterial leg ulceration. |
References:
- Guest, Julian F. Cohort Study Evaluating the Burden of Wounds to the UK’s National Health Service in 2017/2018: Update from 2012/2013. BMJ 2020; 10(10); 1
- Ibid: 1
- Briggs, Shiu-Ling, Leg Ulcer Management: How Addressing a Patient’s Pain can Improve Concordance. Wounds UK 2007; 2
- Newton, Heather. Leg Ulcers: Differences Between Venous and Arterial. Wound Essentials 2011; 6: 20
- Newton, Heather. Leg Ulcers: Differences Between Venous and Arterial. Wound Essentials 2011; 6: 20
- Ibid: 20-1
- Shepherd, John T. Role of the Veins in the Circulation. Circulation Volume 1966; 33: 484
- Davies, Judy et al., Improving the Calf Pump Using Home-Based Exercises for Patients with Chronic Venous Disease. Wounds UK 2008; 4(3): 48
- Hinton, Robert B., Yutzey, Katherine E. Heart Valve Structure and Function in Development and Disease. Annu Rev Physiol 2014; 73: 29-46
- Tobon, Jeniffer et al., Nutritional Status and Wound Severity of Overweight and Obese Patients with Venous Leg Ulcers. J Vasc Nurse 2008; 26(2): 43-4
- Cope, Graham. The Effects of Smoking on Wound Healing. Wounds UK 2014; 10(2): 10
- Newton, Heather. Leg Ulcers: Differences Between Venous and Arterial. Wound Essentials 2011; 6: 22
- Tucker, William D et al. Anatomy, Blood Vessels. StatPearls 2022. Anatomy, Blood Vessels – PubMed (nih.gov)
- Ibid
- Aydin, Ani. Lower Extremity Ulcers: Venous, Arterial, or Diabetic. Emergency Medicine 2009: 18
- Grey, Joseph E et al., Venous and Arterial Leg Ulcers. BMJ 2006; 332(7537): 347-8
- Ibid: 348-50
Resources:
Product website:
Other related articles:
Disclaimer:
Please note that while every effort is made to ensure the accuracy of the content presented, it is purely for educational purposes only and is not a substitute for professional medical advice.